How to Overcome PTSD from Bipolar Disorder
Living with bipolar disorder is not just about navigating mood swings. The emotional wreckage that follows — the fear, guilt, flashbacks, and shame — can feel just as heavy. Many people quietly live with PTSD from bipolar disorder, haunted by what happened during manic or depressive episodes. This overlap between bipolar disorder and PTSD is more common than many realize.
I recently met an old friend who told me that he had overcome cancer a few years ago. He shared with me that even after overcoming cancer, he still lives with PTSD caused by the difficulty of enduring such suffering. It reminded me of what I mentioned in my own book about how I, too, had to heal from the trauma of experiencing mania and depression. But then I looked at him and said, “There is nothing quite like a severe chronic illness that will lead to clarity about the priorities in life.” His head nearly fell off in agreement…
The truth is: the trauma that comes after bipolar episodes is real. You can heal from it, and doing so begins with understanding what your mind and body have endured. But boy, once you’re done with the healing process, life is truly beautiful knowing what really matters.
For more, check out my book The Five Pillars of Bipolar Recovery, book and masterclass. You can also check out my free resources.
What Causes PTSD from Bipolar Disorder?
When you live through extreme mood episodes, your brain and body experience a kind of storm — and sometimes, it leaves scars. Many people develop bipolar disorder trauma or bipolar and PTSD symptoms after severe manic or depressive phases.
Common sources of trauma after bipolar episodes include:
- Losing control during mania or psychosis
- Involuntary hospitalisations or restraints
- Regret and shame from manic behaviours
- The deep isolation of depression
- Rejection or stigma from friends and family
- Fear of relapse and losing control again
These are not overreactions — they’re natural human responses to overwhelming experiences. After my manic episode and year-long severe depression, I gained some footing. What made recovery difficult was my fear of relapse. I was so scared of going back to a bad place that it would ironically trigger PTSD and bipolar anxiety. Recognising that what I was experiencing was a trauma response was the first step toward healing. Ask yourself — is this happening to you?
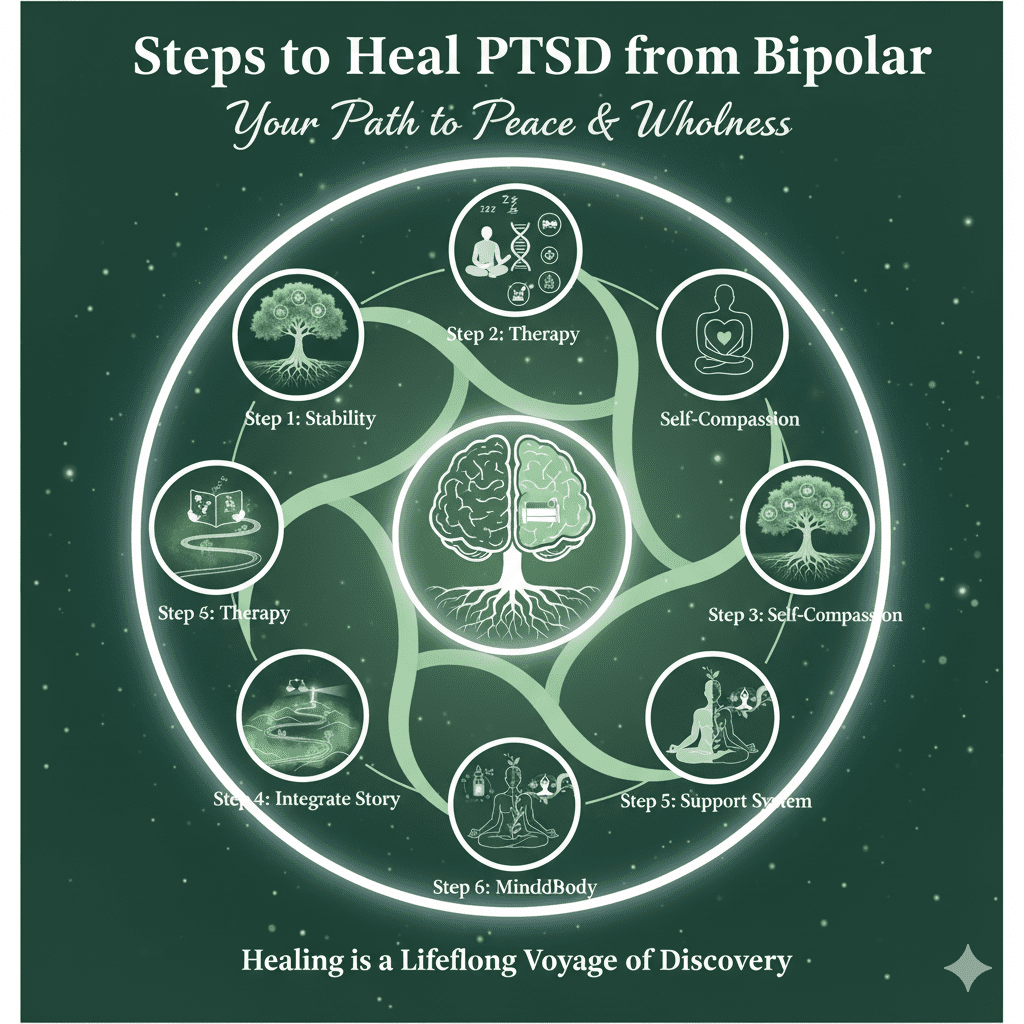
Here are some steps to consider when grappling with the PTSD caused by bipolar disorder.
Step 1: Create Stability Before Healing the Trauma
Before you can process painful memories, your body and mind need safety. For anyone with bipolar disorder and PTSD, this means first focusing on stabilizing mood.
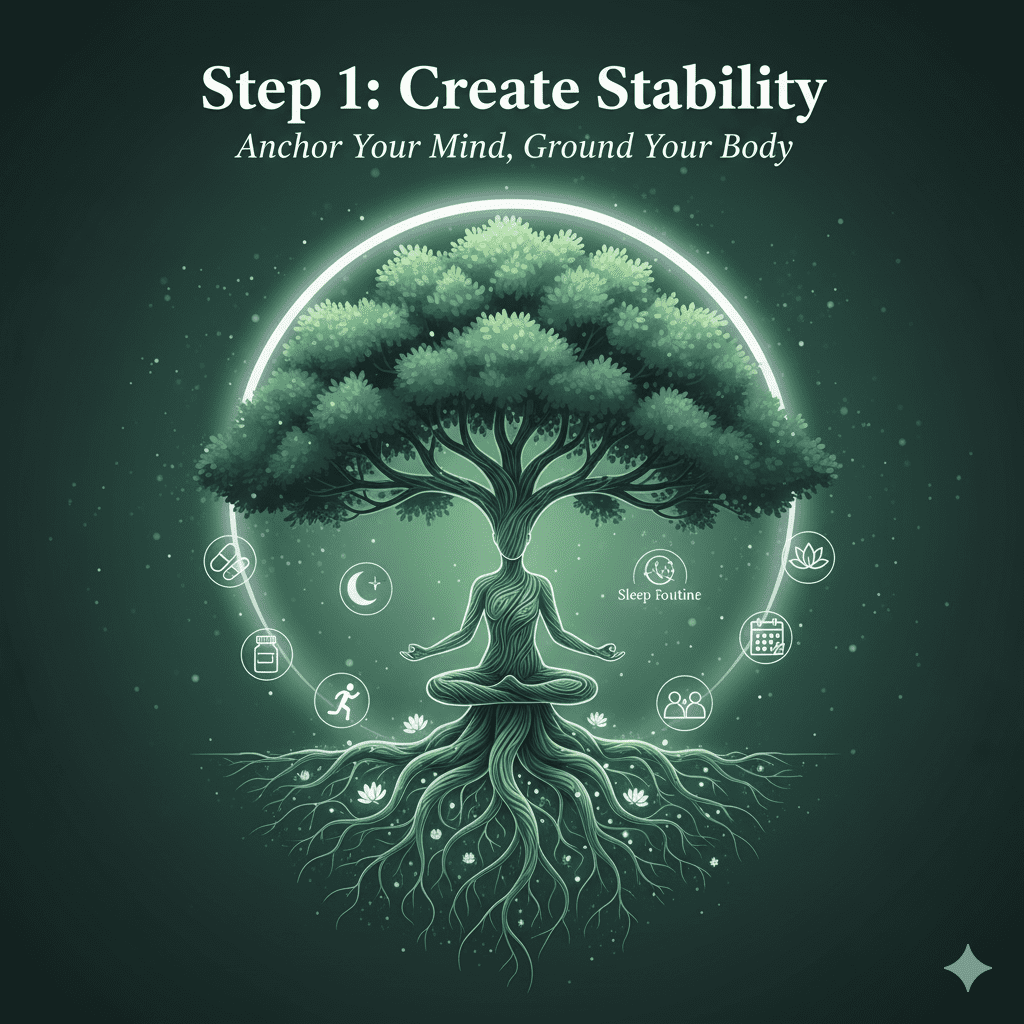
Try to:
- Stay consistent with medication under your psychiatrist’s guidance
- Keep regular sleep and meal routines
- Add exercise to your routine. Walking 2–3 times a week for 20 minutes each is a good way to start if you don’t already have one
- Continue therapy sessions even when you feel “fine”
- Consider learning meditation and finding a wellness community like a yoga studio or rock climbing gym
- Track triggers, early warning signs, and stress patterns — identify what causes the PTSD bipolar depression response
When your body feels safe, your brain can finally begin to let go of the trauma. For me, when I had a poor night’s sleep, I would feel triggered. So I started working with a Cognitive Behavioral Therapist to correct my thinking whenever I felt even slightly off.
Step 2: Work with a Trauma-Informed Therapist Who Understands Bipolar Disorder
Not every therapist understands the interplay between bipolar and trauma. Look for someone who specialises in both.
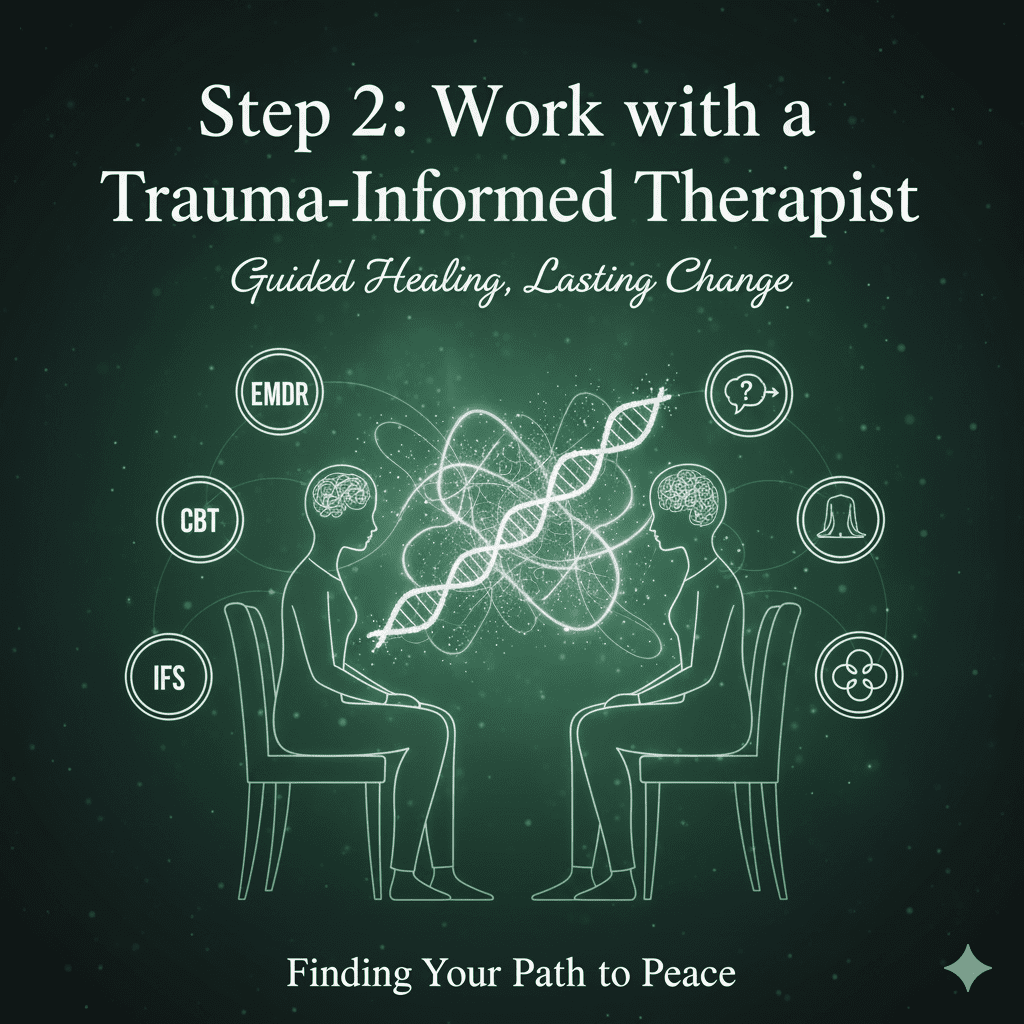
Effective approaches for healing PTSD and bipolar depression include:
- EMDR (Eye Movement Desensitization and Reprocessing) — helps reprocess memories from manic or depressive episodes
- Trauma-Focused CBT — teaches you to challenge guilt and catastrophic thinking
- Somatic Therapies — reconnect you to your body and reduce trauma responses
- Internal Family Systems (IFS) — integrates different “parts” of yourself — manic, depressed, and balanced — into harmony
When reaching out to therapists, ask:
“Do you have experience working with trauma in people with bipolar disorder?”
This ensures you find someone equipped to help you process safely and effectively. Although I am not a therapist, I have worked with dozens of people as an integrative-mental health coach to holistically overcome the acute phases of bipolar disorder and its aftermath. Psychology Today is a great resource to find the right therapist for you.
Step 3: Rebuild Self-Trust and Compassion
After a manic or depressive episode, many people struggle with deep self-blame — common in both PTSD and bipolar disorder:
- “I ruined everything.”
- “Why am I such a failure?”
- “I can’t trust myself again.”
But remember — what happened was not a moral failure. It was a neurological and psychological event that overwhelmed your system. Healing means learning to see your story through the lens of compassion, not shame.
Practical steps:
- Journal your experiences without judgment.
- Replace guilt with understanding: “I was doing my best with the awareness I had.”
- Practice daily affirmations like “I am not my illness — I am the one healing from it.” Check out more affirmations here.
Self-compassion is not indulgence — it’s medicine for the wounded parts of you.
Step 4: Integrate the Past Into Your Life Story
The goal of recovery isn’t to erase the past, but to make peace with it. You survived something extraordinary — and you can learn from it. You WILL learn from it and come out stronger than ever.
Ways to integrate your story:
- Write your bipolar journey as a healing narrative
- Speak about your experiences in a support group
- Use creativity or advocacy to transform pain into purpose — that’s what I did by creating BP Harmony!
When your bipolar and PTSD trauma becomes something you hold — rather than something that holds you — you reclaim your power. Trust me, the more you talk it out to yourself with compassion and to someone who knows how to listen well, the faster you will move toward overcoming bipolar disorder trauma.
Step 5: Strengthen Support Systems and Grounding Practices
Both PTSD and bipolar disorder thrive in isolation. Building a strong network of support is crucial for long-term healing.
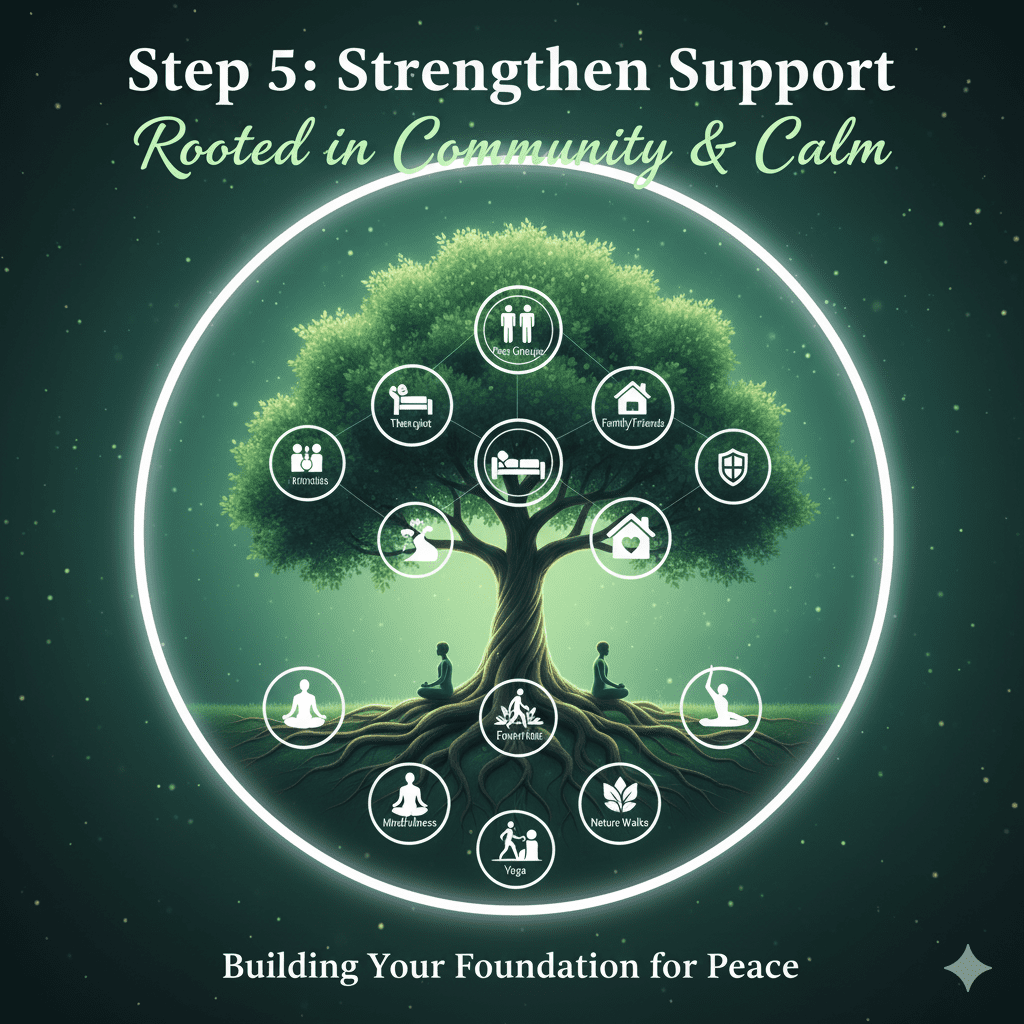
Here’s how to do it:
- Connect regularly with your psychiatrist and therapist
- Join peer groups for bipolar or trauma recovery
- Create a crisis plan for early mood warning signs
- Use grounding exercises like walking, yoga, or prayer
- Spend time walking in nature, which can calm the nervous system and restore balance
Your community can be your mirror — reflecting your growth, not your illness. My fear had to do with judgment because I did in fact face rejection from people who saw me as a liability… and that hurt. The great thing about that time is that it filtered out all the wrong people in my life and made way for so many beautiful people.
Step 6: Medication and Mind-Body Healing
A combination of medication and holistic healing often works best for bipolar disorder and PTSD. Mood stabilizers such as lithium, lamotrigine, risperidone, or valproate can help prevent bipolar depression and PTSD episodes. As always, seek the advice of a licensed health professional when it comes to medications.
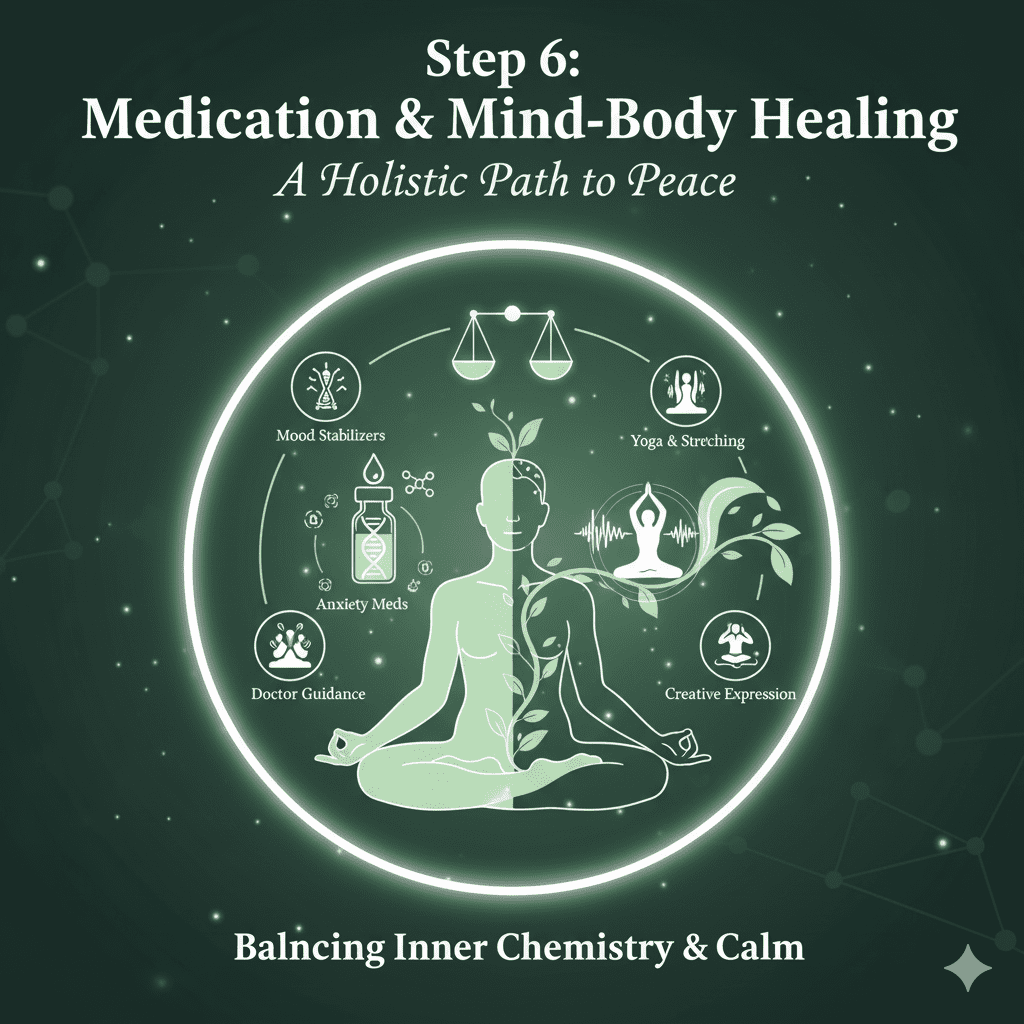
For trauma symptoms like flashbacks or anxiety, psychiatrists may carefully use additional medications, though antidepressants require close monitoring to avoid triggering mania.
Mind-body approaches that support healing include:
- Mindfulness and breath-work
- Gentle yoga and stretching
- Body scanning for tension release
- Creative expression through art, writing, or music
Healing trauma is as much about calming the body as it is about understanding the mind. I love talking about this kind of stuff on my YouTube channel, so check it out to learn more about the mind-body connection.
Step 7: Healing Is a Journey — Not a Destination
My healing journey continues to this day and will continue until my last breath. Recovering from PTSD caused by bipolar disorder takes time, patience, and self-kindness. You might take two steps forward and one step back — and that’s okay.
Every time you choose compassion over shame, or stability over chaos, you are healing.
Every time you tell your story instead of hiding it, you are healing.
And every time you forgive yourself for simply being human, you are already free.
Frequently Asked Questions About Bipolar Disorder and PTSD
1. Can you have both bipolar disorder and PTSD at the same time?
Yes, many people live with both bipolar disorder and PTSD. The two conditions can overlap because traumatic experiences—such as hospitalization, manic episodes, or childhood trauma—can trigger symptoms of post-traumatic stress disorder. Having both PTSD and bipolar disorder can make mood regulation and emotional recovery more complex, but with therapy, medication, and support, healing is absolutely possible.
2. What causes PTSD from bipolar disorder?
PTSD from bipolar disorder often develops after distressing manic or depressive episodes. Experiences like losing control, being hospitalized, or feeling rejected can leave emotional scars. These moments can create bipolar disorder trauma, leading to flashbacks, guilt, or fear of relapse. Recognizing these responses as trauma rather than weakness is the first step to healing.
3. How do I know if I have PTSD or bipolar disorder—or both?
While bipolar disorder affects mood cycles (mania, hypomania, and depression), PTSD involves re-experiencing traumatic memories, hypervigilance, and emotional numbness. If you notice symptoms from both—such as mood swings along with trauma flashbacks or anxiety—it’s important to talk to a trauma-informed therapist who understands both bipolar and PTSD. They can help you clarify your diagnosis and design a treatment plan.
4. How is PTSD from bipolar disorder treated?
Treatment for PTSD and bipolar depression often combines therapy, medication, and lifestyle stability.
- Therapies like EMDR, trauma-focused CBT, or somatic therapy help reprocess traumatic memories.
- Medication may include mood stabilizers for bipolar symptoms and specific treatments for trauma or anxiety.
- Mind-body approaches—such as yoga, mindfulness, and journaling—also support recovery.
Working with a bipolar disorder trauma specialist can make the healing journey smoother and safer.
5. Can trauma make bipolar disorder worse?
Yes. Trauma and bipolar disorder influence each other. Stressful or traumatic experiences can worsen mood instability and increase the risk of manic or depressive episodes. Likewise, living through intense mood swings can cause new trauma. Addressing both conditions together—rather than separately—is key to full recovery.
6. How long does it take to recover from PTSD caused by bipolar disorder?
There’s no fixed timeline. Healing from PTSD caused by bipolar disorder is deeply personal and depends on factors like the severity of trauma, support systems, and treatment consistency. With steady therapy, medication, and self-care, many people notice improvements within months, but emotional integration and self-trust can take longer. Remember: healing is not a race—it’s a journey.
7. Can childhood trauma lead to bipolar disorder?
Research suggests that childhood trauma and bipolar disorder are linked. Early life stress or abuse can increase vulnerability to mood disorders and trauma responses later in life. Understanding this connection can help in developing compassion toward yourself and focusing on trauma-informed bipolar recovery strategies.
8. What are some grounding techniques for bipolar and PTSD recovery?
Grounding practices help manage anxiety and flashbacks common in bipolar with PTSD. Try:
- Deep breathing or 4–7–8 breathing techniques
- Naming five things you can see, four you can touch, three you can hear
- Gentle movement like yoga or walking
- Mindful journaling
These exercises calm the nervous system and build resilience during PTSD and bipolar recovery.
Final Reflection
If you’ve experienced trauma after bipolar mania or depression, know this: you are not broken — you are healing from something that would shake anyone. Your life didn’t end with your episode. It’s being rewritten — one calm breath, one kind thought, one day at a time.
Recovery is possible. You can live a full life again — even after bipolar disorder and PTSD.


