Calming the Mind When You Are Sick: A Mindfulness Practice for Cold, Cough, and Fever
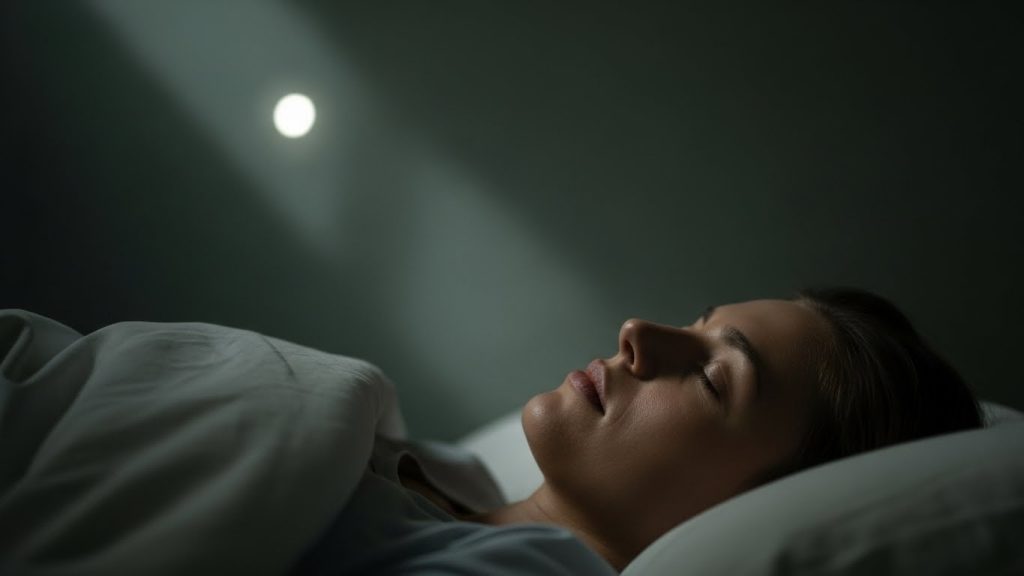
Calming the Mind When You Are Sick: A Mindfulness Practice for Cold, Cough, and Fever Being sick is not only a physical experience. It is also an emotional and mental one. When the body is uncomfortable, the mind often becomes restless, frustrated, and overwhelmed. Simple symptoms such as a cold, cough, or fever can make nights feel long, heavy, and exhausting. Sleep becomes difficult, thoughts become louder, and patience becomes shorter. This mindfulness practice is designed to help you feel emotionally supported while your body is healing. It does not replace medical care, but it offers a gentle way to calm the mind, reduce emotional stress, and create space for rest and recovery. The Emotional Experience of Being Unwell Illness often makes us feel weak, dependent, and out of control. Even mild sickness can affect mood, confidence, and emotional stability. The discomfort of the body can quickly turn into irritation, sadness, fear, or hopeless thinking. It is important to remember that these emotional reactions are natural. The body is under strain, and the nervous system is sensitive. Mindfulness helps us respond to this state with compassion instead of resistance. Separating Identity from Illness One of the most helpful shifts during sickness is learning to separate who you are from what your body is experiencing. You are not your symptoms. You are not your fever, your cough, or your weakness. These are temporary conditions of the body, not definitions of the self. When we say, “My body is sick,” instead of “I am sick,” the mind begins to soften. This language reduces emotional heaviness and prevents the illness from taking over the entire sense of identity. Creating a Safe Space for Healing Rest is the foundation of recovery, but rest is not only physical. The mind must also feel safe. Choose a comfortable position. Dim the lights. Reduce noise and stimulation. Allow the body to be supported. These small adjustments tell the nervous system that it is safe to relax. Using Breath to Calm the Nervous System Slow and conscious breathing helps the body move out of a stress response and into a healing state. When the breath becomes steady, the heart rate slows, muscle tension reduces, and the mind becomes clearer. Take slow, gentle breaths. Allow the belly to rise and fall. Do not force the breath. Let it be soft and natural. Bringing Kind Awareness to the Body As you rest, gently notice the areas of discomfort. There is no need to analyze or fix them. Simply acknowledge their presence. Imagine offering comfort to these areas, just as you would comfort a child who is unwell. Attention itself is soothing. The body often relaxes when it feels noticed and cared for. Working with Difficult Thoughts During Illness Sickness often brings discouraging thoughts. Worries about recovery, frustration with weakness, and impatience with the body are common. When these thoughts arise, gently remind yourself that this is a temporary phase. The body is doing its best to heal. There is no need to fight the experience. Softening the mind supports the body. Allowing Emotions Without Judgment Emotions may surface while you are unwell. You may feel sad, irritable, anxious, or helpless. These emotions do not need to be pushed away. Allow them to exist without labeling them as wrong. Emotions, like symptoms, pass in their own time when they are met with understanding. Supporting Rest and Sleep When You Are Sick Sleep may come in short or broken periods. That is okay. Even moments of quiet rest are beneficial. Lying down, closing the eyes, and breathing calmly supports the healing process. Let go of the pressure to sleep perfectly. Focus instead on resting deeply. The Healing Power of Self-Compassion Being kind to yourself during illness is one of the most important aspects of recovery. Speak to yourself gently. Lower expectations. Allow the body the time it needs. Self-compassion reduces emotional stress, which in turn supports physical healing. Returning to Health With Patience Recovery is not a race. Each body heals at its own pace. Trust the process. Continue to rest, hydrate, follow medical advice, and support your mind with calm awareness. Final Thoughts on Healing the Mind While the Body Recovers Illness reminds us of our vulnerability, but it also offers an opportunity to practice care, patience, and presence. When the mind is calm, the body is better able to heal. May you find comfort, rest, and gentle healing during this time.